Occipital Nerve Block
Head pain is one of the most common pain conditions. The vast majority of people of all ages worldwide have experienced at least a few hours of head pain in their lifetime. But what about head pain that settles in the back and top of your head that becomes chronic? And what happens when this pain is unrelieved by common, over-the-counter medications? For this type of head pain, an occipital nerve block can help. Here’s what you need to know.
What is an occipital nerve block?
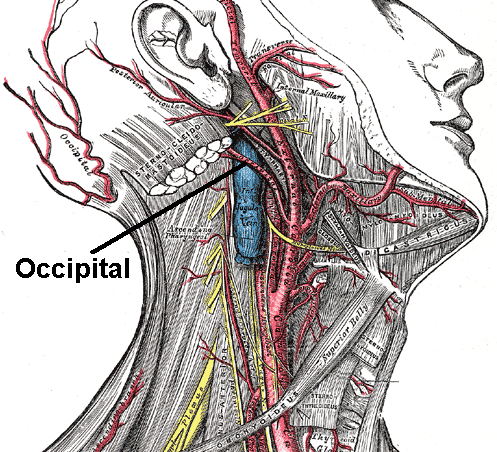
Your greater occipital nerve originates in the second and third vertebrae in your neck, also known as the cervical spine. This group of nerves brings sensation to the back and top of your head.
When the occipital nerve is compressed or injured, pain sensations can stretch from the back of your head to the sides and even around the eyes. Damage to the occipital nerve can be one of the major causes of migraines and chronic headaches.
An occipital nerve block uses an anesthetic and corticosteroid to numb the greater and lesser occipital nerves. The anesthetic relieves pain, and the corticosteroid reduces inflammation.
Occipital nerve blocks can also be a helpful diagnostic tool. If a block does not relieve head pain, then your doctor will know to search for other possible causes of your head pain.
How can an occipital nerve block help me?
These nerve blocks are most often used to treat two main conditions: occipital neuralgia and cervicogenic headache.
Cervicogenic headaches
Cervicogenic headache is another chronic condition. This type of headache may begin to build over a period of time and is not necessarily a result of trauma.
There are a variety of causes of cervicogenic headaches. Some patients with cervicogenic headaches have spondylosis (age-related deterioration in the neck). Others have damage in the cervical facet joints in the neck. In this case, a cervical facet joint injection may be necessary to completely alleviate their symptoms.
But there is research on the successful treatment of cervicogenic headache with occipital nerve block. Study participants who received occipital nerve block found the following positive outcomes:
- Reduced analgesic consumption
- Shorter duration of headache
- Fewer headaches
- Reduction in nausea and vomiting
- Reduced photophobia (fear of light) and phonophobia (fear of noise)
- Increased appetite
- Better quality of life and resumption of activities
Occipital neuralgia
Occipital neuralgia is a condition that usually follows trauma to the nerves in the back of the head (known as the occiput). This type of pain typically occurs as a direct result of trauma (e.g., a blow to the head) and is felt all across the region the occipital nerve enervates.
According to research, occipital nerve blocks can reduce pain scores for six months after treatment for some patients.
What are occipital nerve block benefits?
There are two major benefits to using this type of block. The first benefit is that it can successfully relieve the pain of previously diagnosed occipital neuralgia and cervicogenic headache.
Next, if you do not already have a diagnosis for your acute or chronic head pain, an occipital block can help. If your pain symptoms improve after the injection, this means that the occipital nerve is the source of your pain.
Usually, a series of block injections is needed to treat the problem adequately. However, the response to the block varies from patient to patient. You may only need one injection for profound pain relief. Other patients might benefit from the addition of treatments like occipital nerve stimulation.
How does an occipital nerve block work?
The occipital nerve block procedure is a minimally invasive injection that is performed on an outpatient basis. To minimize your discomfort, your doctor applies a local anesthetic to the injection site before completing the injection. If you are nervous about the procedure, your doctor may provide you with a mild sedative beforehand.
Once you are comfortable, your doctor will place the injection into the greater and lesser occipital nerves. They will inject an anesthetic, a corticosteroid, or both to control pain and inflammation in the nerve.
The procedure itself takes just about 15 minutes. Many patients feel pain relief immediately, but it may take a few days to feel the full effects.
Risks
Occipital nerve block injections are considered generally safe. As with every medical procedure, though, there are associated risks, side effects, and possible complications.
With nerve blocks, the most common side effect is superficial pain from the scalp where the needle was inserted. This pain comes after the local anesthetic wears off but is temporary and typically mild.
Another frequent side effect is bleeding. The scalp has very thin skin with many tiny blood vessels near the surface. Any puncture can result in a dramatic resulting blood flow, but this is common, easily stopped, and temporary. This risk is significantly reduced if ice is placed at the injection site immediately after the procedure.
Other less common risks involve excessive bleeding, infection, and nerve damage.
Patients with an allergy to any of the anesthetics used, or those who are on blood thinning medications, have an active infection, or are pregnant should consult with their pain physician before receiving the procedure.
Recovery
Recovery from an occipital nerve block is fast and generally pain free. You may experience mild pain at the injection site, but this is temporary and should be mild. Return to regular activity as pain levels allow, or when your doctor okays it.
If you do not experience pain relief, or symptoms worsen, call your doctor.
References
- Occipital nerve blockade for cervicogenic headache: a double-blind randomized controlled clinical trial Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tawfik OM. Pain Pract. 2006 Jun;6(2):89-95 PMID: 17309715
- Repetitive occipital nerve blockade for cervicogenic headache: expanded case report of 47 adults. Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tawfik OM. : Pain Pract. 2006 Dec;6(4):278-84 PMID: 17129309
- Greater occipital nerve injection in primary headache syndromes–prolonged effects from a single injection Afridi SK, Shields KG, Bhola R, Goadsby PJ. Pain. 2006 May;122(1-2):126-9. Epub 2006 Mar 9 PMID: 16527404
- Textbooks: Atlas of Interventional Pain Management Author(s): Waldman, Steven D. Pub. Date: 7/1/1998 Publisher (s): Elsevier Science Health Science division.