Interscalene Block
The effects of a shoulder injury and trauma can ripple across your life. Starting with the initial injury or pain, when everyday tasks are challenging, all the way through the intense recovery after shoulder surgery, it’s important to have proper pain relief and support. An interscalene block can help you work towards recovery with powerful, post-surgery pain relief. Here’s what you should know about this pain management approach.
What is an interscalene block?
An interscalene block offers pain relief during or after shoulder surgery.
During shoulder surgery, general anesthesia provides most of the pain relief. After surgery, nerve blocks can be used for pain relief. This relief helps you to begin physical therapy and other treatments to speed the healing process. Why is this tool so important?
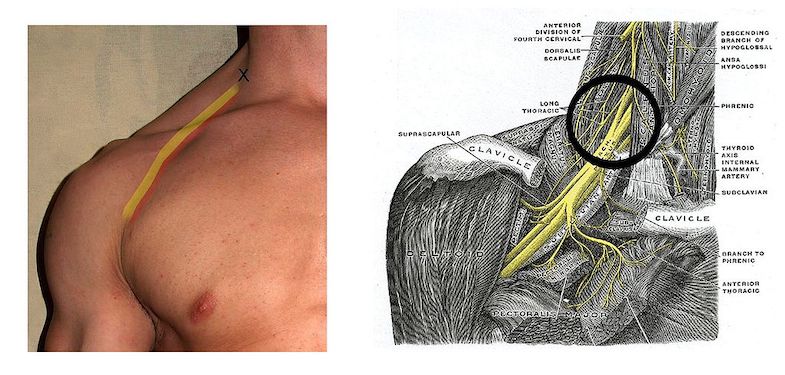
Your shoulder is host to a system of nerves called the brachial plexus. This system of nerves is responsible for sensation and motion in the shoulder, upper arm, forearm, and hand. The brachial plexus moves between two muscles on the side of your neck: the anterior and medial scalene muscles. In an interscalene block, a painkiller is injected within the area near the brachial plexus.
An interscalene block temporarily disrupts sensation and movement to this area. As a result, interscalene blocks can provide pain relief during or after surgery on the shoulder, clavicle, upper arm, or elbow. This is especially helpful while undergoing physical therapy or recovering after surgery.
Do note that because pain relief is inconsistent and may not be enough during the actual surgery, an interscalene block is not appropriate for forearm or hand surgery.
How can an interscalene block help me?
An interscalene block can be used to treat the following injuries or conditions:
- Humerus fracture
- Acromioplasty
- Rotator cuff repair
- Total shoulder replacement
- Hemiarthroplasty
- Most other arm surgeries involving the outside edge of the forearm or hand
These surgeries often come with significant amounts of pain, but surgery is just the beginning of healing. One of the complicating factors in a full recovery from shoulder surgery is inactivity. Excessive pain after surgery can limit activity, which can lead to further complications (e.g., frozen shoulder). An interscalene block is also particularly helpful with the rehabilitation process, providing pain relief while you work on re-building your range of motion and strength.
How does the interscalene block procedure work?
The interscalene block procedure can be performed while you’re awake or under general anesthesia. If you are feeling anxious about the procedure, small doses of sedative can be given before, during, and after the block.
Your doctor will settle you on an examination table on your back with your head turned away from the area to receive the block. Some doctors may use nerve stimulation or other imaging techniques to target the correct placement of the block before proceeding.
The area to be injected will be cleaned and sterilized completely before your doctor injects an anesthetic that works to block pain and motor signals to the brain.
You may receive the interscalene block on the side of your neck either towards the front of your body or towards the back. The injection should block the shoulder muscles, including the deltoid, infraspinatus, supraspinatus, and teres major.
An interscalene block generally lasts less than a day. This may seem like a short period of time, but it is usually enough to either supplement pain medications during surgery or to allow for extra pain relief directly after.
Risks
Generally, interscalene blocks are considered safe, but as with any medical procedure it’s important to identify possible complications. Complications of interscalene block may include hematoma, infection, and allergic reaction.
Other complications are more specific to the procedure. These include:
- Abnormal skin sensation (parasthesias)
- Anesthetic systemic toxicity
- Diaphragmatic paralysis
- Hoarseness
- Horner syndrome
- Collection of air in the chest causing the collapse of a lung (pneumothorax)
Horner syndrome consists of contraction of pupil (miosis), drooping upper eyelid (ptosis), and an inability to sweat (anhidrosis).
Talk to your doctor about your concerns and any previous complications from surgery or anesthesia you have experienced. They can assess your unique risk profile.
Recovery
When interscalene blocks are administered on their own, the recovery period is brief, as the block typically lasts just one day. It is important to have someone drive you home from the procedure and to take a day to rest.
When they are conducted as part of another surgery, your recovery may take as long as it takes to recover from surgery. Talk to your doctor about your specific recovery plan, and follow all of their directions, especially regarding activity levels and pain medications.
Shoulder injury and treatment both involve a long and sometimes-painful path to healing. Interscalene blocks can be one part of a comprehensive approach to rehabilitation of your shoulders and arms after surgery.
Get in touch today to learn more about how this block can help you.
References
- Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology. 2002;97(5):1274-80.
- Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. 2001;95:875-80.
- Hortense A, Perez MV, Amaral JL, Oshiro AC, Rossetti HB. Interscalene brachial plexus block. Effects on pulmonary function. Rev Bras Anesthesiology. 2010;60:130-7.
- Liu SS, Gordon MA, Shaw PM, Wilfred S, Shetty T, Yadeau JT. A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth Analg. 2010;111(3):617-23.
- Muhly WT, Orebaugh SL. Sonoanatomy of the vasculature at the supraclavicular and interscalene regions relevant for brachial plexus block. Acta Anaesthesiol Scand. 2011;55(10):1247-53.
- Stone MB, Wang R, Price DD. Ultra sound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26(6):706-10.
- Swenson JD, Bay N, Loose E, Bankhead B, Davis J, Beals TC, Bryan NA, Burks RT, Greis PE. Outpatient management of continuous peripheral nerve catheters placed using ultrasound guidance: an experience in 620 patients. Anesth Analg. 2006;103:1436–1443.
- Winnie A: Plexus Anesthesia; Vol 1: Perivascular techniques of brachial plexus blocks. Philadelphia, WB Saunders Co, 1984.