Piriformis Syndrome
Maybe it starts as a dull ache in your buttock or hip when you stand up from sitting for too long or when you are climbing stairs. Perhaps sciatic pain that radiates down your leg begins to occur more regularly, making it harder and harder to get comfortable in any position. If your pain persists and continues to worsen, you may have piriformis syndrome. Here’s what you need to know.
What is piriformis syndrome?
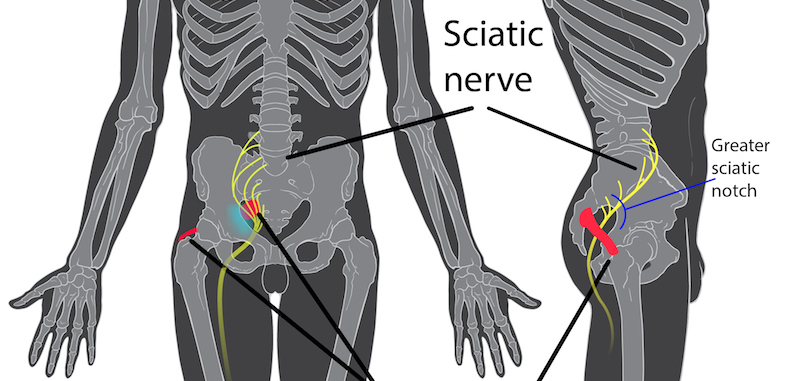
Piriformis syndrome is a condition in which the piriformis muscle compresses the sciatic nerve. This compression causes pain to travel through your buttocks to the side and back of the leg and down to the foot, often accompanied by tingling or numbness. This type of radiating pain is called sciatica. Sciatic pain may be most often associated with a herniated disc, but it can also occur with piriformis syndrome. This type of pain is a symptom of the condition, not a condition in and of itself.
Piriformis syndrome pain begins with muscle tension and spasms that affect the sciatic nerve. Most patients report an ache deep in the buttocks, which is intensified by sitting or climbing stairs.
Other than sciatic pain, piriformis syndrome symptoms also include:
- Numbness in the feet
- Pain walking up a hill
- Headache
- Weakness in the legs
- Reduced range of motion in the hips and leg
- Pain in the abdomen, pelvis, or groin
- Back pain during bowel movements
- Pain during sexual intercourse (for women)
The intensity of piriformis symptoms varies wildly from person to person depending on their age, activity level, and any comorbid conditions. Some people may only have mild, annoying symptoms, while others may be completely debilitated.
Further, piriformis syndrome can be an acute condition that resolves with rest, or a chronic, debilitating problem resistant to treatment.
What causes piriformis syndrome?
The piriformis muscle makes walking and your overall balance possible. It’s a large, flat, pyramid-shaped muscle deep underneath the gluteal muscles in the buttocks. Starting at the sacral spine, the piriformis muscle travels to the greater trochanter of each femur, stabilizing the hip and allowing the thigh to move outward from the body. In most people, the sciatic nerve rests underneath the piriformis muscle, but in about 15% of the population, the sciatic nerve passes through the muscle.
Regardless of where the sciatic nerve travels, the most common cause of piriformis syndrome seems to be overuse or improper use of the piriformis muscle. This can lead to inflammation in the muscle, which then compresses the sciatic nerve. Any injury or trauma to that area of the body can also cause inflammation that leads to nerve compression.
Repetitive motions performed during activities such as running or lunging stress the piriformis muscle, causing contractions that apply pressure to the sciatic nerve. Certain activities can irritate the piriformis, including:
- Prolonged sitting
- Climbing stairs
- Squatting
- Running uphill
Compression of the sciatic nerve can result in inflammation that exacerbates pain, leading to a chronic condition. Although sciatic pain is equally possible in men and women, piriformis syndrome is more common in women than men.
Certain chemicals may also cause inflammation that, when combined with other factors, can lead to piriformis syndrome. These chemicals include histamine, serotonin, prostaglandin, and bradykinin.
Comorbid conditions
Patients affected with Morton’s neuroma may also be at increased risk for developing piriformis syndrome. This condition involves an anatomical deformity of the second metatarsal that destabilizes the foot during walking, resulting in internal rotation of the leg. The piriformis compensates by contracting repetitively during the push-off phase of walking, which can cause chronic compression of the sciatic nerve.
Other conditions that may result in piriformis syndrome include:
- Cerebral palsy
- Total hip arthroplasty
- Pseudoaneurism in the inferior gluteal artery near the sciatic nerve
Do I have piriformis syndrome?
A definitive test for piriformis does not exist, so a diagnosis is made based on a detailed history and physical exam. Your doctor will ask questions to find out when your pain began, how long it lasts, and what makes it worse.
It can be very helpful to keep a pain journal when you first notice symptoms. Record any instances of pain and note:
- Activity level (before and after pain)
- Duration and severity
- Characteristics of pain (e.g., numbness, sharp, dull ache, etc.)
Keeping a pain journal offers more insight into potential causes of your pain as well as aids in diagnosis.
By palpating the piriformis, your doctor may determine if it is contracted and tense. The Freiberg test determines involvement of the piriformis muscles with a simple movement. When forced internal rotation of the extended leg results in pain in your buttocks or down the leg, piriformis syndrome is a strong possibility.
Another movement that contracts the piriformis muscle selectively is the Beatty maneuver. Lie on the side that is not in pain, bend the knee towards the chest, and then pressing the knee down towards the ground. This activates the piriformis and, when piriformis syndrome is present, results in pain.
A visual exam can also show shortening of the leg on the affected side. You may also have a splayed foot on the affected side when lying on your back.
An X-ray or MRI does not diagnose piriformis syndrome but can rule out other, more common causes of sciatica, such as:
- Herniated spinal discs
- Fibrous adhesions of other muscles in the area surrounding the sciatic nerve
- Hamstring tendinitis
Nerve conduction tests may be helpful in excluding other conditions as well.
What piriformis syndrome treatments could help me?
In the acute stages of piriformis syndrome, first-line treatment focuses on resting the muscle, avoiding activities that aggravate pain, and pain relief measures. Pain management after the first 24 hours may utilize heat. A heating pad placed on the muscle for 20 minutes at a time may reduce inflammation and pain.
Other treatments include:
- Physical therapy: A physical therapist can offer stretching exercises that relax the piriformis muscle and reduce pressure on the sciatic nerve. These stretches involve moves that flex and adduct the hip.
- Massage: Massage speeds up the healing process by increasing blood flow to the inflamed area and reducing or preventing muscle spasms. Your doctor may prescribe muscle relaxers or anti-inflammatory medications for short-term relief.
- Acupuncture: Acupuncture can decrease tension in the body.
- Biofeedback: Biofeedback training helps to control the body’s physical response to pain
- Simple stretches: Yoga and other types of mild, low impact exercise can help in healing and preventing further injury.
Interventional approaches
For persistent pain that does not respond to conservative treatment options, corticosteroid and anesthetic injection to the area may reduce inflammation and pain.
Surgery is an extreme measure only taken as a last resort in treating chronic, debilitating pain.
References
- Mayo Clinic. (April 22, 2010). Sciatica. Retrieved from http://www.mayoclinic.com/health/sciatica/DS00516/DSECTION=prevention
- John P. Revord, MD. (April 8, 2000). What is Piriformis Syndrome? Retrieved from http://www.spine-health.com/conditions/sciatica/what-piriformis-syndrome
- The Piriformis Syndrome. (February 1997). Retrieved from http://www.rice.edu/~jenky/sports/piri.html
- Milton J Klein, DO, MBA. (July 10, 2012). Physical Medicine and Rehabilitation for Piriformis Syndrome. http://emedicine.medscape.com/article/308798-overview